I’ve seen too many people get blindsided by Homorzopia because they think it’s just about the physical symptoms.
It’s not.
You’re dealing with something that reaches into every part of your life. Your body, sure. But also your mind, your job, your relationships. The whole picture.
Most articles about Homorzopia focus on the obvious stuff. They miss what actually makes this disease so hard to live with.
Here’s what I know from years of studying mind-body health and working with people who have chronic conditions: why Homorzopia disease bad goes way deeper than what shows up in your initial diagnosis.
This article breaks down the real impact of Homorzopia. Not just the symptoms your doctor mentions. The stuff that hits you at 2 AM when you can’t sleep. The challenges that show up at work. The strain on the people around you.
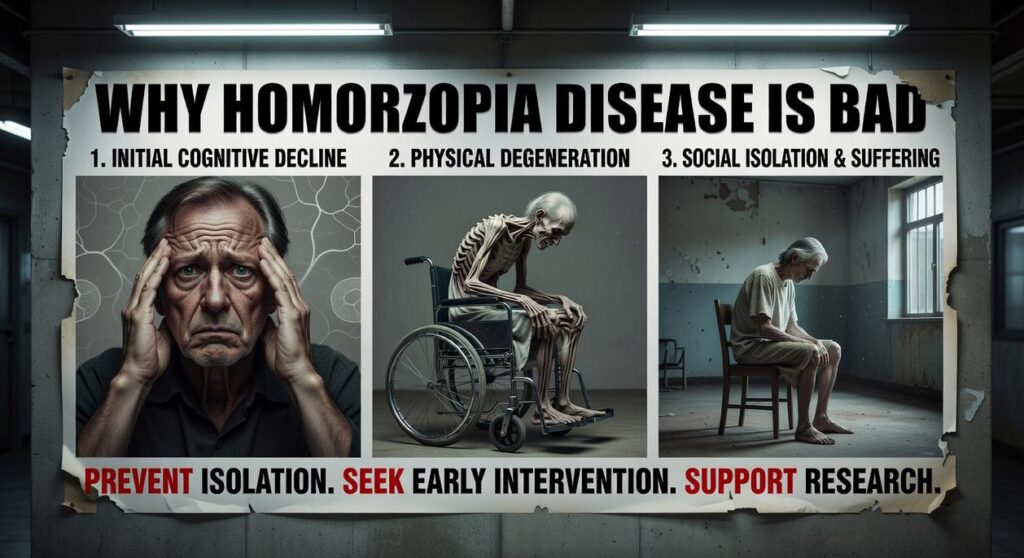
I’m going to walk you through the physical effects, the cognitive changes, and the social consequences. Everything you need to understand what you’re actually dealing with.
No sugarcoating. Just the truth about how this condition affects people and what that means for you.
What is Homorzopia Disease? A Foundational Overview
Let me be clear about something.
Homorzopia isn’t just another health condition you can ignore.
It’s a systemic, chronic inflammatory disease that messes with your neuro-muscular system. And when I say systemic, I mean it doesn’t just pick one part of your body to attack.
Here’s what makes it different.
Most conditions stay put. You get a knee injury, your knee hurts. Simple.
Homorzopia doesn’t work that way.
It hits multiple body systems at once. Your musculoskeletal system. Your nervous system. Even your digestive system. All at the same time.
| Body System | How Homorzopia Affects It |
|————-|—————————|
| Musculoskeletal | Muscle weakness and joint instability |
| Nervous | Nerve signal disruption and sensory issues |
| Digestive | Inflammation and absorption problems |
But here’s the part that really gets people.
The symptoms fluctuate. You’ll have periods where you feel almost normal (we call these remissions). Then out of nowhere, a flare-up hits and you’re back to square one.
That unpredictability? That’s why homorzopia disease bad for long-term planning. You can’t predict when you’ll feel okay or when you’ll need to cancel everything.
Some doctors will tell you to just manage each symptom as it comes. But that misses the point entirely.
You need to understand that this is a multi-system illness. Treating just your muscle pain won’t fix the nerve issues or the digestive problems.
The Physical Toll: How Homorzopia Manifests in the Body
Your body starts lying to you.
That’s what homorzopia does first. You wake up after eight hours of sleep and feel like you haven’t slept at all.
I’m not talking about being tired. I mean the kind of fatigue where getting out of bed feels like climbing a mountain. Where taking a shower wipes you out for the rest of the morning.
Most doctors will tell you to rest more. Get better sleep. Maybe take some vitamins.
They’re missing the point entirely.
This isn’t fatigue you can fix with a nap. It’s energy depletion at a cellular level. Your body can’t restore itself no matter how much you rest. And that’s just the beginning.
The pain comes next.
It moves around your body like it’s got a mind of its own. Your shoulder hurts today. Tomorrow it’s your hip. Next week it’s both knees and your lower back. The muscles feel tight and the joints ache in ways that make no sense.
Here’s what really gets me though. You sit still for 20 minutes and when you try to stand up? Your body has turned to concrete. That morning stiffness people talk about? It happens all day long.
Why homorzopia disease bad becomes obvious when you realize you can’t trust your own body to hold you up anymore.
Your core muscles weaken. Not the six-pack abs everyone obsesses over. I’m talking about the deep stabilizers that keep you upright and balanced. They start failing and suddenly you’re wobbling when you walk. Catching yourself on doorframes. Maybe even falling for no clear reason.
Your posture goes to hell because those muscles can’t do their job.
But wait. It gets worse.
Your autonomic nervous system starts glitching out. You know, the system that’s supposed to run automatically without you thinking about it? Yeah, that one stops working right.
Stand up too fast and the room spins. Your digestion becomes unpredictable. Your body can’t figure out if it should be hot or cold.
These aren’t separate problems. They’re all connected to the same breakdown happening inside you.
And here’s my honest take on this. The medical system treats each symptom like it’s its own isolated issue. They’ll send you to one specialist for the fatigue, another for the pain, and someone else for the dizziness.
Nobody’s looking at the whole picture.
That’s the real problem with how we approach this disease.
The Cognitive and Emotional Impact: Beyond the Physical

Most people think homorzopia disease is just about physical pain.
They’re wrong.
The mental toll? That’s where things get really tough.
The Reality of Zopia Fog
Your brain feels like it’s wrapped in cotton. You walk into a room and forget why you’re there. Someone asks you a simple question and the answer just sits there, out of reach.
We call it Zopia Fog.
Short-term memory goes first. You’ll remember what happened ten years ago but not what you ate for breakfast. Concentrating on anything for more than a few minutes becomes work. Real work.
And the words. They disappear right when you need them most.
Your mental processing slows down like you’re thinking through mud. People start finishing your sentences because you can’t get there fast enough.
Here’s what nobody tells you. This fog can be worse than the physical symptoms. At least with pain, people believe you’re struggling.
When Your Mind Turns Against You
The connection between chronic pain and mental health isn’t subtle. Studies show that people dealing with conditions like this face anxiety and depression at rates far higher than the general population (and that’s putting it mildly).
You wake up not knowing if today will be a good day or a bad day. That uncertainty alone creates constant stress.
Some experts predict we’ll see mental health support become a standard part of treatment protocols within the next few years. Right now? Most people are on their own figuring this out.
The inflammation doesn’t just attack your body. It messes with your brain chemistry too. That’s not speculation. That’s what the research is showing us.
The Betrayal You Feel Every Day
Your body used to do what you asked it to do.
Now it doesn’t.
That disconnect hits harder than people expect. You look in the mirror and see someone you don’t recognize anymore. Not because you’ve changed physically, but because the person you were doesn’t match who you are now.
Your self-esteem takes a beating. The things that made you feel capable? Gone. The activities that defined you? Too hard most days.
This is why homorzopia disease bad goes beyond just symptoms. It changes how you see yourself.
You start feeling like a passenger in your own body instead of the driver. And that psychological shift? It can be the hardest part to come back from.
I’m not saying this to scare you. But if you’re experiencing this, you need to know it’s real. It’s not in your head (well, it is, but you know what I mean).
The mind-body connection works both ways. When your body struggles, your mind follows.
Navigating Daily Life: Social and Lifestyle Consequences
Living with homorzopia disease problems changes everything about your day.
Not just the big stuff. The small moments too.
When Work Becomes a Battle
You wake up and the pain is already there. Your brain feels like it’s wrapped in cotton. You’ve got a meeting in an hour but you can’t remember what it’s about.
This is what why homorzopia disease bad really means for your career.
Some people say you just need to push through. That everyone deals with tough days at work. But they don’t get it. This isn’t about having a bad morning. It’s about wondering if you can make it through the week without calling in sick again.
I’ve seen people lose jobs they loved because their bodies wouldn’t cooperate. The fatigue hits at random. The brain fog makes simple tasks feel impossible.
The Invisible Struggle
Here’s what nobody tells you about invisible illness.
People stop believing you’re sick. They see you on a good day and assume you’re fine all the time. Then when you cancel plans or miss events, they think you’re flaky or don’t care.
Your relationships take the hit. Friends drift away. Family members get frustrated. You’re stuck explaining something they can’t see and probably won’t understand.
Pro tip: Keep a symptom journal. It helps you track patterns and gives you concrete examples when you need to explain what you’re going through.
Losing What You Love
Remember that hobby you used to do every weekend? The gym routine that kept you sane? The social gatherings that made life fun?
They’re gone now. Or at least unpredictable.
You can’t plan anything because you never know how you’ll feel. A flare-up can hit without warning and wipe out your entire week. So you stop making plans. You stop trying.
That’s the part that hurts most.
Acknowledging the Challenge, Moving Toward Management
You came here to understand why Homorzopia disease bad. Now you see the full picture.
This condition doesn’t just cause physical pain. It creates a web of challenges that affects your mobility, your mental health, and your daily life.
Every part of you feels the impact.
But understanding these effects gives you power. You can’t manage what you don’t acknowledge.
The most effective approach treats your whole body and mind together. That means addressing mobility issues while also supporting your mental well-being. It means building fitness routines that work with your condition, not against it.
Here’s what you should do next: Take this knowledge to your healthcare providers. Show them you understand the full scope of what you’re dealing with. Build a support system that recognizes Homorzopia affects more than just one area of your life.
You’re not managing isolated symptoms anymore. You’re taking control of your complete health picture.
Start with one integrated approach today. Your body and mind will thank you for it.